By Shelly Gordon
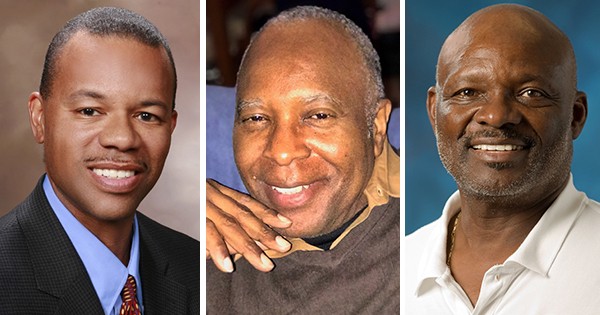
Reggie Dye, Thomas Newell, and Victor Murray
Nationwide — Three African American men: Reggie Dye, a healthcare executive, Thomas Newell, a retired basketball referee for youth at risk and Victory Murray, NASA lead engineer whose team repaired Apollo 13, wanted a better way to treat their prostate cancer—one that promises a better quality of life post-treatment than surgery and radiation which are the standards of care. These two procedures can come with a greater risk of urinary incontinence, erectile dysfunction and penile shrinkage.When diagnosed with localized prostate cancer, they each selected a noninvasive procedure called High Intensity Focused Ultrasound (HIFU). They got together to share each of their stories about their HIFU treatment, which is widely used across the world, but still relatively new in the United States, with select physicians across the country delivering the treatment.
HIFU is a noninvasive focal-therapy procedure that destroys targeted prostate tissue. HIFU directs extremely precise high-frequency sound waves that heat up and burn off only the diseased portion of the prostate, sparing surrounding tissue and nerves. Therefore, risks of common side effects associated with surgery and radiation — urinary incontinence and erectile dysfunction — are lessened with HIFU.
African American Men at Higher Risk for Prostate Cancer
According to the American Cancer Society, African American men are 1.5 times more likely to be diagnosed with prostate cancer than white men, and twice as likely to die from the disease. In fact, the risk of African American men dying from low-grade prostate cancer is double that of men of other races, according to a study in the Journal of the American Medical Association (December 2019).
In light of those statistics, a study in Cancer, a peer-reviewed journal of the American Cancer Society (ACS) recommends that black men be screened for prostate cancer more often and at a younger age. The study is significant because it challenges the conventional wisdom that early screening of typically slow-growing prostate cancer can lead to over-treatment.
Prostate Cancer Treatments – Standard of Care & HIFU
For decades, doctors have offered prostate cancer patients two choices for treatment: radiation or radical surgery to remove the entire prostate, which can cause those life-altering side effects and compromise their quality of life. More recently over the past decade, men with less aggressive disease have had the option to choose active surveillance. But for some of those men, going to bed each night knowing they have cancer in their bodies that could progress negatively affects their peace of mind.
Dye, Newell and Murray each chose the HIFU procedure because the risks of urinary incontinence and erectile dysfunction were less likely to occur than with surgery or radiation.
“I’m very glad I chose HIFU for my prostate cancer treatment,” Murray said. “I also consider myself lucky because I was diligent about receiving my annual physical, and I feel honored to share my challenge with prostate cancer.”
“My advice to other men – especially African American men who are at even greater risk — is to find a physician you trust and heed the professional advice you are given. I hope in some small way I can encourage someone else who may be reluctant to get the right treatment to become a prostate cancer survivor. I did with the help of my doctors and HIFU!”
Murray, Newell and Dye share their stories: Why they each chose HIFU, its impact on their lives, and why they encourage their peers to get tested early and often. Find their video here.
Shelly Gordon is the founder of G2 Communications. For more than a dozen years, Shelly has worked with a variety of medical specialists and medical device manufacturers across the U.S., and has written numerous articles about medical conditions and treatments that have appeared in top healthcare publications in print and online.
PRESS CONTACT:
G2 Communications
sgordon@g2comm.com
